Fecal microbiota transplantation in MS?
Fecal microbiota transplantation in MS?
A disbalance in the gut microbiome may play a role in the pathogenesis of multiple sclerosis. Microbiome modifying therapies can therefore be an interesting area for novel MS treatment. Although probiotics and dietary changes have not shown to be effective, researchers have been speculating about fecal microbiota transplantation as a new therapy.
Another disease in which the microbiome plays a crucial role in its pathology is Clostridium difficile infection (CDI). This disease can arise when the gut microbiota has been disturbed, mostly by antibiotics. [1] Patients who have recurrences in this disease can have a very high disease burden. For some of these people fecal microbiota transplantation (FMT) may be an outcome. [2] A randomized controlled trial has shown the effectiveness for fecal microbiota transplantation in recurrent CDI. [3] Today, the only indication for a fecal transplantation are recurrent CDI. Considering the fact that in MS patients the microbiome is also altered, FMT might have potential as a novel treatment in multiple sclerosis.
In fact, a fecal microbiota transplant has been performed in a patient with MS in Calgary, Canada [4]. The FMT, of which her partner was the donor, was given because she was also suffering from recurrent CDI. The case describes a 61-year old female patient with secondary progressive MS. This patient had already been suffering from MS for approximately 30 years. Before she received the transplant she was no longer suffering from relapses, but she did worsen in her EDSS. The Expanded Disability Status Scale describes the limitation in function of patients with MS on a scale from zero (normal neurologic examination) to ten (death due to MS). Because her balance, lower limb power and bladder function (for example) diminished, her EDSS increased from 2 to 6 within 5 years. Around this time, she additionally developed recurrent C difficile infections for which she received FMT. After this her EDSS did not increase further and stayed stable over the next ten years.
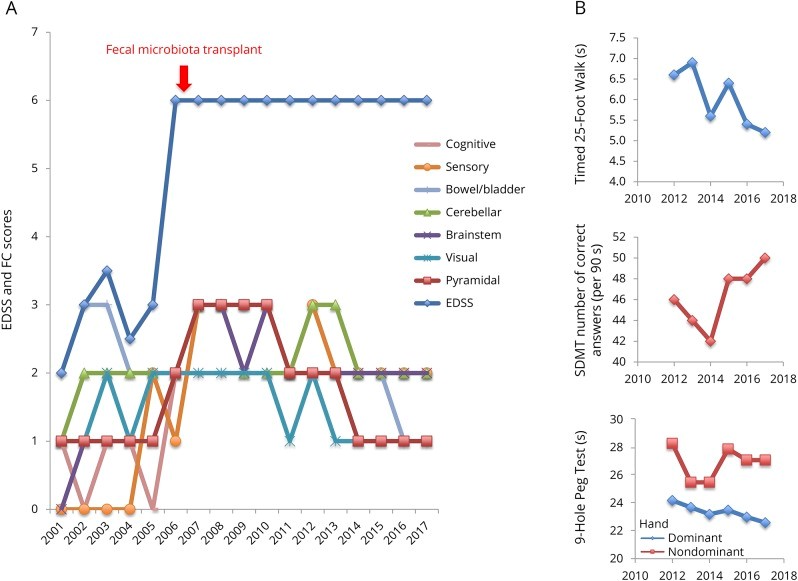
Image 2. These graphs show the scores measured in this patient case.
A. This graph shows the EDSS and FSS during a ten year follow up. It clearly shows stabilization of the EDSS after fecal microbiota transplant administration, no additional treatment of therapy was given to achieve this result. The 7 Functional System Score subject are also shown of which most points are slightly improved.
B. From 2012 the MSFC scores were routinely measured at her clinic. These scores include measurement of leg function/ambulation, cognitive function and arm/hand function (in B. from above to below). All three have improved from 2012 till end of the follow up.
The researchers explain that the recurrent C diff. infections created an inflammatory response which most likely caused the fast worsening in the disease. After adjusting her misbalance in gut bacteria the worsening of neurological symptoms (EDSS) stabilized. It is a shame that in this case the microbiome of the patient was not researched in different timepoints, like before C. diff infection and after FMT. A longer follow-up would be very interesting to see whether symptoms will return. Because her previous microbiome and the microbiome after transplantation are unknown, the pathway by which the FMT had effect in this patient is only speculation. Clinical trials are necessary to evaluate the possibility of using this novel therapy in MS.
There are a few initiatives to perform trials like this. One example is a phase-2 trial with forty participants being performed in London. [5] They will be divided into two groups of twenty patients. The first group will receive the FMT at the start while the second group will provide as a control group in the first six months. The second group will also receive the FMT after this period. This study is estimated to be completed this December (2018). Another initiative is by the Nederlandse Donor Feces Bank (NDFB) [6] in the Netherlands, in collaboration with different Dutch medical centers. The NDFB is an initiative of doctors and researchers. Their goal is to improve the availability of FMT for recurrent C diff infections in the Netherland. This group is still in a design-phase, trying to figure out how the ideal study on FMT in MS patients should be performed. So far, fecal microbiota transplantation is only indicated to recurrent C diff infections.
Altogether, the microbiome has an important
role in teaching our immune system and keeping a healthy gut environment.
Disbalance in the composition of gut bacteria is called dysbiosis and may be a
key factor in the development of several disease. The possible role of the gut
bacteria dysbiosis in MS pathogenesis has led to much interest in microbiome
modifying therapies. Fecal microbiota transplantation seems to be a promising
possibility in therapy development for multiple sclerosis.
Written by Jip de Weijer
Posted on 14 oct 2018
[1] Rijksinstituut voor Volksgezondheid en Milieu. Clostridium difficile - LCI richtlijn. Available via: https://lci.rivm.nl/richtlijnen/clostridium-difficile
[2] Gupta S. et al. Fecal microbiota transplantation: in perspective. Therap Adv Gastroenterol (2016)
[3] Van Nood E. et al. Duodenal infusion of donor feces for recurrent Clostridium difficile. N Engl J Med, 368 (2013)
[4] Makkawi S. et al. Fecal microbiota transplantation associated with 10 years of stability in a patient with SPMS. Neurol Neuroimmunol Neuroinflamm (2018)
[5] Kremenchutzky M. Fecal microbial transplantation in relapsing multiple sclerosis patients. In: ClinicalTrials.gov. Available at: clinicaltrials.gov/ct2/show/NCT03183869
[6] Nederlandse Donor Feces Bank. FMT voor andere aandoeningen dan Clostridium difficile infecties? Available at: www.ndfb.nl
Image 1: copied from Proto Magazine; Bright Future for the Feces cure (https://protomag.com/articles/bright-future-feces-cure). This material is protected by
copyright law and available for personal, non-commercial use only.
Image 2: Makkawi S. et al. Fecal microbiota transplantation associated with 10 years of stability in a patient with SPMS. Neurol Neuroimmunol Neuroinflamm (2018)

